Sygeplejersken
Active involvement of elderly surgical orthopaedic patients in their own dietary care increases postoperative energy and protein intake
In this study the individual patient has been actively involved in his own dietary care and has contributed to finding solutions that increase their dietary intake. Hospitalised patients have to a greater extent chosen their own food and drinks from the daily menu. The results show that they chose food and drinks that were rich in energy and protein. This also includes energy- and protein-enriched drinks.
Sygeplejersken 1999 nr. 21, s. 36-44
Af:
Preben Ulrich Pedersen, sygeplejerske, ph.d.,
Ulla Cameron, sygeplejerske,
Lisbeth Jensen, klinisk diætist

After undergoing a major operation many elderly patients are at risk of becoming undernourished. Insufficient intake of energy and protein results in loss of muscle tissue, leading to an increase in fatigue and in the frequency of complications as well as a prolonged rehabilitation period.Objective: To demonstrate whether energy and protein intake in elderly surgical orthopaedic patients is increased if they become actively involved is their own dietary care during hospitalisation.
Patients: The study involved patients 65 years or over who were consecutively admitted for surgery for a fractured neck of femur or for hip- or knee alloplasty at Roskilde County Hospital, Køge. Patients with dementia, cancer, liver-, kidney- or endocrine disorders were excluded.
Design: Study procedure. The daily energy and protein intake was recorded following the ward's normal routine in 135 patients. Intervention was carried out in 107 patients. The result of intervention was determined by comparing the intake of energy and protein in the two groups.
Intervention: The approach was based on Salling's nursing model. During the admission interview the primary nurse systematically determined the patients' energy and protein requirements, their eating problems and habits as well as their need for nursing care at meal times. The results of the daily recordings of dietary intake were presented to the patients in the form of a bar chart, which served as the basis for continued dialogue.
Variables: Energy and protein intake, weight and height, number of interviews.
Results: Intake of energy and protein rose by 25 per cent and 50 per cent respectively. Obese patients increased their intake of protein without increasing their intake of energy. The number of patients consuming less than 33 per cent of their requirements was significantly reduced.
Conclusion: Patients who became systematically involved in their own dietary care increased energy and protein intake during hospitalisation regardless of gender, age, or patient classification (elective/emergency). The method facilitated the early identification of patients with poor appetite and the initiation of appropriate measures.
Introduction
During illness many patients experience difficulty in satisfying their bodies' requirements for energy and protein (1). Whilst in hospital both medical and surgical patients are at risk of being malnourished (2-7), with elderly patients in particular at risk of developing protein-energy malnutrition (PEM) (8-10).
Insufficient nutrition following an operation can complicate the patient's recovery, prolonging hospitalisation and the rehabilitation phase, even leading to death in extreme cases (8,11,12). The immune system is weakened by further risk of infection (13) and delay in wound healing (14,15), while weight loss leads to increased fatigue (16,1), thus weakening the patient's ability not only to complete a rehabilitation programme but also to stay active (1,16,18).
A great number of factors adversely affect the patient's nutritional intake. Nursing staff have no systematic procedure for identifying patients with nutritional problems and are thus unable to uncover the cause of this malnutrition. Consequently, appropriate and necessary intervention fails to take place (19,21). The planning of meal times with too few staff at hand to provide assistance and too little time to eat (10,21,22) inhibits intake. Similarly, the food portions served by staff can be characterised more by the staff's appetite than the patient's desire for food (10). Patients with eating disorders can avoid eating if food is served as a sit-down meal and they cannot live up to the norms concerning table manners, hygiene and behaviour (10). Poor sitting posture whilst eating (22), impaired chewing ability (23), unappetising food (21,24), lack of knowledge about suitable diet (25), and the absence of genuine choices can also
Side 37
affect nutritional intake. Finally, the surroundings where the food is eaten might also exert a powerful influence on how much is eaten (26,27).
These factors leading to malnutrition could all be addressed by introducing a higher degree of individualisation into hospital feeding within the framework that exists at each institution. If the patient is actively involved in the feeding process, this will undoubtedly help in solving health-related problems (28,29). The purpose of this investigation is to demonstrate that energy and protein intake in elderly surgical orthopaedic patients increases if they become actively involved in their own dietary care during their hospital stay.
Materials
The study was carried out at surgical orthopaedic ward H, Roskilde County Hospital, Køge from 7 November 1995 to 15 March 1997. A total of 369 patients who were consecutively admitted for elective hip/knee alloplasty or emergency surgery for a fractured neck of femur, and who were all over 65 years of age, able to understand Danish and expected to be in hospital more than 7 days, were invited to take part in the study. Of these patients, 17 declined, 37 were not able to understand the information given, 26 were already receiving dietary treatment, and 16 suffered from cancer, gastrointestinal disorders or were undergoing treatment with steroids. In addition, 5 patients were unable to take part due to serious uncompensated heart disorders, 11 were transferred to intensive/cardiac units after their operation and did not return to the surgical orthopaedic ward, while 4 more patients were prevented from participating for orther reasons. Altogether, 253 patients took part in the study.
Design
The study was quasi-experimental in design and took the form of a controlled study procedure without randomisation, where the patients were blind to the intervention. Energy and protein intake were recorded in both the control group, which followed the standard meal routines of the ward, and the intervention group, which was subjected to the new meal routines of the ward. The effect of the new routine was measured by comparing the dietary intake of both patient groups. The patients hospitalised from 7 November 1995 to 30 June 1996 were allocated to the control group, while patients hospitalised from 1 September 1996 to 31 March 1997 were allocated to the intervention group.
Intervention
The intervention was based on stimulating the patients to independently increase their energy and protein intake. In order to achieve this, Salling's humanistically-inspired nursing model (29) was used. The model refers to motivation and development theories described by Murray, Maslow and Piaget, where nursing actions should focus strongly on actively incorporating the patients and their personality into the care. This stimulates the individual's personal activity both during hospitalisation and after discharge (30).
The nursing model necessitates the completion of an admission interview, daily interviews with the patient in conjunction with the primary nurse scheme, which involves the same nurse throughout the hospital stay (29-30).
In this study the admission interview was defined as a dialogue in connection with drawing up a dietary journal, with continued dialogue in the form of daily interviews about how the patient's current nutritional requirements were being met. Information, guidance and instruction were given in conjunction with the interviews.
The continuity of the interviews was ensured by the presence of a project nurse, who acted as a primary nurse for nutrition for alle the patients.
In the primary nurse's absence, the interviews were conducted by the research coordinator. The elective patients in the intervention group were each sent a leaflet one month prior to admission containing information on preoperative dietary advice, and all patients completed a dietary journal on admission into the hospital.
Throughout the hospital stay, this journal lay by the patients' bed and contained information about their eating problems and habits, need for nursing care at meal times as well as a chart of the patient's energy and protein intake together with information regarding diet and operation. The course of the daily interviews was determined by the results of the previous day's dietary record. The patients received individual guidance on how to sensibly put together the next day's meal based on their wishes and availability. The difference in nursing care given to the control and intervention groups is illustrated in Table
1.
Side 38
During the interviews there was no discussion of rehabilitation problems, which if raised were instead referred to other staff on the ward. No change was made in relation to the ward menu, its nutritional value or the ward's rehabilitation process during the period of the study.
Dietary journal
Dietary intake was recorded from 7:00am to 7:00am, commencing from the 1st whole postoperative day to the last day before discharge, up to a maximum of 20 days. The patient and/or the nursing staff recorded the food and fluid intake on a regular basis. Each morning the entries were reviewed together with the patient to prevent errors.
The record of dietary intake assumed that patients were served the hospital's standard portions, and that both patients and staff were able to assess the amount of food eaten. There was a strong correlation between the portions served and the size of the standard portion (r=0.88), between the information given by patients about what they actually ate (r=0.95) and a high level of consistency amongst the staff's estimates about what was eaten (k=0.80) (31).
The testing of the dietary recordings indicated a high level of reliability. Energy and protein intake in the diet was calculated by the clinical dietician on the ward according to the hospital's standard recipes. Data was entered into a computer programme, specially designed for this study (32,33).
The dietary intake was related to the patient's requirements and presented in a bar chart, showing how much of the energy and protein intake was met by the current dietary intake.
Table 1. Nursing care given to control and intervention patients
|
ACTIONS |
STANDARD CARE |
INTERVENTION CARE |
|
CONTROL PATIENTS |
INTERVENTION PATIENTS |
|
|
Systematic completion of admission interview on eating habits and problems |
No |
Yes |
|
Systematic calculation of energy and protein requirements |
No |
Yes |
|
Daily recording of the dietary intake |
Yes |
Yes |
|
Daily assessment of the need for nursing care in connection with the dietary intake |
No |
Yes |
|
Systematic help with eating problems |
No |
Yes |
|
Systematic information, guidance and instruction about sensible eating in connection with an operation |
No |
Yes |
|
Implementation of the primary nurse scheme for nutrition |
No |
Yes |
Measurement of energy and protein requirements
Energy and protein intake was measured in accordance with the Danish national recommendations (34). The calculation of the energy requirement was achieved by multiplying the Basal Metabolic Rate (BMR) with an activity, stress or weight gain factor. The BMR was set to 100kj/kg bodyweight. Activity factor: in bed = 1.1, upright = 1.3. Stress factor: long bone fractures and major operations = 1.3; temperature increase = 1.2. Weight gain factor: underweight = 1.3 (BMI<20). The energy requirement was adjusted daily in accordance with the above factors. The protein requirement (34,35): 1.5g/kg bodyweight.
Side 39
At BMI>25 1.5g/kg of the highest limit for normal weight, equivalent to BMI=25.
Table 2. Patient profile in the control and intervention groups
|
CONTROL PATIENTS |
INTERVENTION PATIENTS |
TOTAL |
||
|
n=135 |
n=107 |
n=242 |
||
|
% |
% |
% |
||
|
Gender: |
Male |
26 |
32 |
29 |
|
Female |
74 |
68 |
71 |
|
|
Patient classification: Emergency |
59 |
53 |
56 |
|
|
Elective |
41 |
47 |
44 |
|
|
BMI on admission: |
||||
|
¡20.0 |
12 |
14 |
13 |
|
|
20.0-25.0 |
38 |
37 |
37 |
|
|
25.1-30.0 |
38 |
36 |
37 |
|
|
¡30.0 |
9 |
13 |
11 |
|
|
Unknown |
3 |
0 |
2 |
|
|
Median age (range) |
76 (65-97) |
76 (65-95) |
76 (65-97) |
Other variables
All patients were weighed on the same scales dressed only in their underwear. Elective patients were weighed the day before operation, with emergency patients on the first occasion they were able to move postoperatively, although no later than the 3rd postoperative day. The patient's height was measured without shoes. The day of the operation was classified as day '0'. The number of continued interviews was recorded.
Ethics
Participation took place following receipt of oral and written informed consent. The study was reported to the Data Surveillance Authority and approved by the Regional Committee on Scientific Ethics for Roskilde County, case number 1995-1-62.
Statistics
Data was processed using the statistics programme SPSS. The T-test for unpaired data was used for normally distributed continuous data. Where data was not normally distributed the Mann-Whitney test was used. The confidence interval (CI) shown by the table (36) was used for nominal and ordinal scaled data.
Results
A total of 11 patients dropped out of the study whilst in hospital, which meant that 242 patients completed the study. Patient composition in the study corresponded to patients in both Roskilde County and the rest of Denmark calculated on an annual basis with regard to gender, age and diagnosis on admission for included and excluded patients. Excluded patients did not differ from the investigated patient group regarding age or gender. There was no difference in composition between the control and intervention group of patients (Table 2).
Admission interviews were carried out in connection with the admission of all intervention patients. In addition, a total of 917 follow-up interviews were conducted with intervention patients during their hospital stay, equivalent to a mean of 8.6 (+/-3.2) interviews per patient.
Diet was recorded in 85 per cent of days when the
Side 40
patient was hospitalised in both the control and intervention group, equivalent to 11,2 (+/-4.2) and 9.6 (+/-3.8) days, respectively.
The patients' mean intake of energy and protein
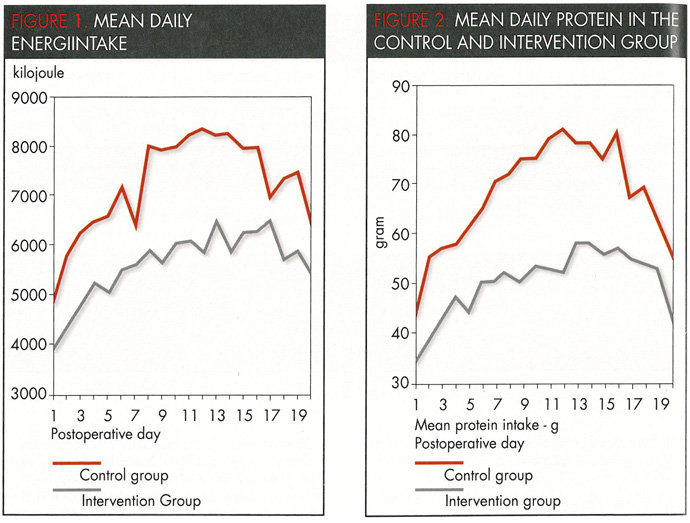
Daily energy and protein intake during hospitalisation for the control and intervention group as 5616kJ (+/-1338) and 6539kJ (+/-1621) per day (p<0.001), respectively, and 47g (+-12.3) and 68g (+/-15.4) protein (p<0.001), respectively. Figures 1 and 2 illustrate the mean daily intake of energy and protein from the 1st to the 20th day in hospital.
Energy intake in the intervention group rose significantly for all patient groups (Table 3). For patients with BMI>30 there was no increase (p=0.2) in the energy intake.
The daily intake of protein rose significantly in the intervention group regardless of BMI. There was no difference in the mean daily intake of energy and protein among the control patients.
The patients' calculated energy and protein requirements during hospitalisation
The mean daily energy and protein requirements calculated were the same for the control and intervention patients, 11,329 kJ (+/-2046) and 11,526 kJ (+/-2082) (NS), respectively, and 95g (+/-13.7) and 95g (+/-16.2) (NS), respectively.
The calculated energy requirements for the control and intervention patients were met in 49 per cent (+/-13) and 58 per cent (+/-16), (p<=.001) of cases, respectively, and for the protein requirements with 51 per cent (+/-14) and 74 per cent (+/-17) (p>=.001), respectively.
Side 41
In total, 29 patients (12 per cent) had an energy intake <35 per cent of their calculated requirements during their stay in hospital. This concerned 20 control patients (15 per cent) and 9 intervention patients (8 per cent) (p<=0.05). There was no difference in the number of patients with poor appetite in relation to gender, age group or patient classification. Two patients with BMI<20 and 27 patients with BMI<20 (>0.01) suffered from poor appetite throughout their hospital stay.
Table 3. Mean energy and protein intake in the control and intervention group according to gender, patient classification, age and BMI
|
CONTROL GROUP KJ |
INTGROUP KJ |
RELATIVE IN- CREASE |
SIGNIFICANCE |
CONTROL GROUP PROTEIN IN G |
INTGROUP PROTEIN IN G |
RELATIVE INCREASE |
SIGNIFICANCE |
|
|
Male |
5496 (1349) |
7163 (1984) |
30% |
p¡0.001* |
48 (13.2) |
73 (19.5) |
52% |
p¡0.001* |
|
Female |
5253 (1335) |
6249 (1339) |
19% |
p¡0.001 |
47 (12.1) |
66 (12.7) |
40% |
p¡0.001 |
|
Emergency |
5178 (1205) |
6521 (1617) |
26% |
p¡0.001 |
45 (11.9) |
67 (15.7) |
49% |
p¡0.001 |
|
Elective |
5517 (1499) |
6559 (1642) |
19% |
p¡0.001 |
49 (12.8) |
69 (15.1) |
41% |
p¡0.001 |
|
65-74 years |
5280 (1666) |
6624 (1820) |
25% |
p¡0.001 |
47 (14.9) |
70 (17.1) |
49% |
p¡0.001 |
|
75+ years |
5340 (1499) |
6482 (1485) |
21% |
p¡0.001 |
46 (10.4) |
66 (14.1) |
43% |
p¡0.001 |
|
BMI |
||||||||
|
¡20 |
5584 (978) |
6555 (1953) |
17% |
p¡0.05* |
48 (9.5) |
62 (17.1) |
29% |
p¡0.01* |
|
20-25 |
5142 (1113) |
6538 (1544) |
27% |
p¡0.001 |
46 (10.9) |
68 (15.0) |
48% |
p¡0.001 |
|
25.1-30 |
5514 (1435) |
6629 (1420) |
21% |
p¡0.001 |
48 (13.6) |
70 (14.1) |
46% |
p¡0.001 |
|
¡30 |
5373 (1477) |
6281 (2082) |
17% |
p=0.2* |
49 (13.2) |
72 (17.7) |
47% |
p¡0.001* |
Figures in () indicate 1 SD standard deviation. Significance is determined using t-test, * using Mann-Whitney's test.
Discussion
With the nursing intervention it has been possible to achieve a dramatic increase in postoperative energy and protein intake in elderly surgical orthopaedic patients. This increase was immediately in evidence from the 1st postoperative day.
The investigated patient group was representative of elderly patients admitted for elective hip and knee alloplasty or emergency surgery for a fractured neck of femur. The patients in the study reflect the number of patients admitted each year in Roskilde County and the rest of Denmark with respect to age and gender.
No changes were made to the hospital menu during the study period. The dietary intake was recorded and calculated in the same way for both patient groups. The dietary journals of the patients in the control group were first assessed at the end of the study. The results were therefore not able to affect the dietary intake of the control group. Elderly patients with a fractured neck of femur had a spontaneous energy and protein intake of between 3800 and 4800 kJ and 27-28g protein/day during hospitalisation. (11,37,38). The control group's intake lay above this, although this might be explained by the presence of a dietary journal scheme that may have increased the attention of the patients and staff to nutrition, subsequently influencing the control group's dietary intake. Another explanation could be that the hospital's menu and eating environment as well as the assistance provided by the nursing staff may have previously been of a higher quality than has been the case in foreign studies.
By systematically giving energy- and protein-enriched drinks to supplement the normal hospital food it has been shown in several intervention studies that the energy intake can increase to 4600-5600 kJ and the protein intake to 40-50g per day (11,37). In this study the energy and protein intake of patients
Side 42
in the intervention group was even greater.
The use of energy- and protein-enriched drinks offers an excellent supplement to hospital food, although it does not eliminate the basic causes behind why patients eat too little. In addition, a large number of patients do not wish to take these drinks (39). It has previously been shown that the motivation in patients to solve a health problem is increased when the patients become actively involved in their own care (28).
In this study the individual patient has been actively involved in his own dietary care and has contributed to finding solutions that increase his dietary intake. Hospitalised patients have to a greater extent chosen their own food and drinks from the daily menu. The results show that they chose food and drinks that were rich in energy and protein. This includes also energy- and protein-enriched drinks.
It has been described earlier that a gradual increase takes place in the dietary intake from the 1st to the 10th postoperative day (38,40). Development in the daily energy and protein intake in the control and intervention group followed the same pattern. Figures 1 and 2 show that the dietary intake rose sharply until the 4th postoperative day in both groups. The dietary intake then stabilised until the 6th and 7th postoperative day when a further increase was noted. Previous studies describing the development of postoperative dietary intake are based on such small material that it is not possible to determine whether stabilisation of dietary intake also occurs on the 5th postoperative day. This study offers no data that could explain this phenomenon. The swings in dietary intake from the 17th to the 20th postoperative day are undoubtedly due to the fact that the overall figures are based only on a few patients, as 85% of the patients had already been discharged before the 16th postoperative day.
Increased postoperative protein intake is of great importance in preventing complications during hospitalisation as well as after discharge (11,41,42), as increased protein intake has shown to be of immense benefit in wound healing, the strengthening of the immune system and preservation of muscle mass (11,43).
In patients with BMI>30, reduced wound healing capability and a lower lymphocyte count can be attributed to the fact that the patients involved had a relatively low protein content in the body (41). The energy intake in the intervention group did not increase in patients with BMI>30. On the other hand, their protein intake rose, as it proved possible to make their diet more balanced in terms of protein.
In patients who have consumed less than 35 per cent of their calculated nutritional requirements over a period of more than 14 days, the initiation of nutritional therapy is recommended, in order to prevent the development of nutrition-related complications (34). This study has, however, demonstrated that the inclusion of patients in their own dietary care results in a decrease in the number of patients with low nutritional intake. This was achieved by identifying such patients soon after admission and ensuring that intervention was initiated directly before any real nutritional therapy proved necessary.
Despite intervention, patients on average only satisfied their requirements for energy and protein by 60 per cent and 75 per cent, respectively. This can be attributed to several factors, including the insufficiency of the hospital menu, overcalculation of energy requirements, and most likely, the inability of patients to ingest the amount of food necessary to meet their calculated requirements for energy and protein. Further studies are necessary to determine how much energy and protein intake is sufficient as well as realistic for patients to consume.
In conclusion, patients who became actively involved in their own dietary care increased energy and protein intake during hospitalisation regardless of gender, age or patient classification. Patients who consumed too little energy and protein in relation to their current requirements were quickly identified and appropriate action taken. In this respect, the described method contributed to revealing the reasons why patients eat too little and to finding solutions which patients believe will alleviate their problems and increase dietary intake.
Undersøgelsen er gennemført som led i et ph.d.-studium ved Forskningsenheden for Klinisk Sygeplejeforskning, Klinisk Institut, Odense Universitet, med professor Anne-Lise Salling Larsen som hovedvejleder. Tak til Sygekassernes Helsefond for økonomisk støtte af undersøgelsen. Endvidere en stor tak til alle medarbejdere på Roskilde Amts Sygehus Køge for engageret deltagelse ved gennemførelsen af undersøgelsen.
Keywords: Elderly, empowering, energy and protein intake, nutrition, postoperative.
Litterature
- Kondrup J, Ovesen LF. Ernæring på sygehuse. Ugeskr Laeger 1997;159(24):3755-9.
- Hessov I. Energy and protein Intake in elderly patients in an orthopaedic surgical ward. Acta Chir Scand 1977;143:145-9.
- Ovesen L, Allingstrup L, Hannibal J, Mortensen EL, Hansen OP. Effect of dietary counseling on food intake, body weight, response rate, survival and quality of life in cancer patients undergoing chemotherapy: A prospective, randomized study. J Clin Oncol 1993;11(10):2043-9.
- Enig B, Winther E, Hessov I. Energy and proteinintake and nutritional status in non-surcigally treated patients with small cell anaplastic carcinoma of the lung. Acta Radiologica Oncology 1986;(25):19-22.
- Bisballe S, Buus S, Lund B, Hessov I. Food intake and nutritional status after gastrectomy. Human Nutrition: Clinical Nutrition 1986;40C:301-8.
- Nielsen K, Kondrup J, Martinsen L, Stilling B, Wikman B. Nutritional assessment and adequacy of dietary intake in hospitalized patients with alcoholic liver cirrhosis. Br J Nutr 1993;69:665-79.
- Jensen MB, Hessov I. Dietary supplementation at home improves the regain of lean body mass after surgery. Nutrition 1997;13:422-30.
- Larsson J, Unosson M, Ek A-C, Nilsson L, Thorslund S, Bjurulf P. Effect of dietary supplement on nutritional status and clinical outcome in 501 geriatric patients a randomised study. Clin Nutr 1990;9:179-84.
- Unosson, M. Malnutrition in hospitalised elderly patients. 1993; Linköping University; 483.
- Sidenvall B. The meal in geriatric care. Habits, values and culture. 1995; Linköping University; 484.
- Delmi M, Rapin C-H, Bengoa J-M, Delmas PD, Vasey H, Bonjour J-P. Dietary supplementation in elderly patients with fractured neck of the femur. Lancet 1990;335:1013-6.
- Sullivan DH. The role of nutrition in increased morbidity and mortality. Clin Geriatr Med 1995;11(4):661-74.
- Clandra RK. Nutrition, immunity, and infections: Present knowledge and future directions. Lancet 1983;26(March):688-91.
- Stotts NA, Washington DF. Nutritions: A critical component of wound healing. AACN 1990;1(3):585-92.
- Schroeder D, Gillanders L, Mahr K, Hill GL. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. JPEN 1991;15(4):376-83.
- Stock SE, Clauge MB, Johnston IDA. Post-operative fatigue a real phenomenon attributable to the metabolic effects on body nutritional stores. Clin Nutr 1991;10:251-7.
- Christensen T, Kehlet H. Postoperative fatigue and changes in nutritional status. Br J Surg 1984;71(June):473-6.
- Christensen T. Postoperative fatigue. 1995; University of Copenhagen; 3 p. 33-5-266.
- Sidenvall B. Long-term care patients and their dietary intake related to eating ability and nutritional needs: nursing staff interventions. J Adv Nurs 1993;18:565-73.
- Abbasi AA, Rudman D. Observations on the prevalence of protein-calorie undernutrition in VA nursing homes. JAGS 1993;41:117-21.
- Kayser-Jones J, Schell E. The effect of staffing on the quality of care at mealtime. Nursing Outlook 1997; 45(2):64-72.
- Keller H. Malnutrition in institutionalized elderly: How and why? JAGS 1993;41:1212-8.
- Dormenval V, Budtz-Jørgensen E, Mojon P, Bruyère A, Rapin C. Nutrition, general health status and oral health status in hospitalised elders. Gerontology 1995;12(2):73-80.
- Clevenger FW, Rodriguez DJ, Demarest GB, Osler TM, Olson SE, Fry DE. Protein and energy tolerance by stressed geriatric patients. J Surg Res 1992;52:135-9.
- Pedersen PU, Cameron U. Ældre ortopædkirurgiske patienters viden om kost, ønsker til måltidsrutiner og ernæringsfremmende aktiviteter under sygehusindlæggelse. Vård i Norden 1998; Accepteret 25.11.98.
- Elmstaal S. Hospital nutrition in geriatric long-stay medicin Dietary intake, body composition and the effects of experimental studies. 1987; University of Lund, Sweden. Dissertation.
- Ragneskog H, Bråne G, Karlsson I, Kihlgren M. Influence of dinner music on food intake and symptoms common in dementia. Scan J Caring Sci 1996;10:10-7.
- Salling Larsen A; Vejleskov H. Patienten som samarbejdspartner. 1. ed. Copenhagen: Dansk Sygeplejeråd; 1985.
- Salling Larsen A. Stimulation af patienters aktivitet og udvikling. 1990; Odense University; Dissertation.
- Salling Larsen A. Klinisk sygepleje. Månedsskr Prak Lægegern 1996;74(Nov.):1253-60.
- Pedersen PU. Stimulation til øget kostindtagelse effekten af at medinddrage patienter over 65 år i egen kostforplejning. 1998; Odense Universitet, Syddansk Universitet; (Under publicering).
- Grønhøj L, Hagen FE, Holdt M, Lindblom J, Meisner E, Taanum C. Informatikkens rolle ved kostregistrering. Aalborg Universitetscenter. 1996.
- Jensen M, Mikkelsen L, Rytter C. 5. semester opgave (ingen titel). Slagelse. Data Skolen i Roskilde. 1996.
- Pedersen AN, Ovesen L editors. Anbefalinger for den danske institutionskost. Copenhagen. Levnedsmiddelstyrelsen & Økonomaskolen i København. 1995;233.485.
- Hessov I. Energi- og proteinbehov hos syge voksne. Näringsforskning 1980;24(3):88-90.
- Diem K, Seldrup J, Lentner C, editor. Introduction to statistics, statistical tables, mathematical formulae. 8. ed. Basle: Ciba-Geigy Limited; 1982.
- Stableforth PG. Supplement feeds and nitrogen and calorie balance following femoral neck fracture. Br J Surg 1986;73:651-5.
- Jallut D, Tappy L, Kohut M, Bloesch D, Munger R, Schutz Y, Chiolero R, Felber J-P, Livio J-J, Jéquier E. Energy balance in elderly patients after surgery for a femoral neck fracture. JPEN 1990; 14(6):563-8.
- Williams CM, Driver LT, Older J, Dickerson WT. A controlled trial of sip-feed supplements in elderly orthopaedic patients. Eur J Clin Nutr 1989;43:267-74.
- Hackett AF, Yeung CK, Hill GL. Eating pattern in patients recovering from major surgery a study of voluntary food intake and energy balance. Br J Surg 1979;66:415-8.
- Gherini S, Vaughn BK, Lombardi AV, Mallory TH. Delayed wound healing and nutritional deficiencies after total hip arthroplasty. Clinical Orthopaedics and Related Research 1993;293:188-95.
- Tkatch L, Rapin C-H, Rizzoli R, Slosman D, Nydegger V, Vasey H, Bonjour J-P. Benefits of oral protein supplementation in elderly patients with fracture of the proximal femur. J Am Coll Nutr 1992;11(5):519-25.
- Hill GL, Douglas RG, Schroeder D. Metabolic basis for the management of patients undergoing major surgery. World J Surg 1993;17:146-53.
